Breastfeeding
Breastfeeding Basics: Getting Started

If feels like there’s so much to learn when becoming a new mom! Pregnancy, birth, breastfeeding—is there ever an end to all the information you’re supposed to process and digest before your baby arrives? You definitely need to take some time just to dream about the little one growing in your womb.
New life is such a miracle! And as far as breastfeeding education goes, relax. We’ve gathered easy-to-follow, step-by-step information for you to read and discuss with your health care provider.
First, remember your body produces milk as a normal part of the reproductive cycle. You don’t have to have any special information to make that happen! But the technique of breastfeeding is a learned skill, and it’s enhanced by practice and support. While you have breastfeeding information prenatally, the opportunity to postnatally practice attaching the baby to the breast and assessing the baby’s breastfeeding effectiveness provides you with confidence as you embark on this particular journey of parenting. Let’s dive into the specifics.
Prenatal breastfeeding management
Mothers often stop breastfeeding earlier than planned due to an unforeseen problem. Mom should have the necessary information to prevent breastfeeding-related problems and to solve them if they occur. A prenatal breastfeeding class provides a foundation for mom and baby to get off to a successful start. Maternal education during pregnancy is also highly recommended for best breastfeeding management. And try watching some breastfeeding videos, reading books, and talking to family and friends. Breast examinations are a great part of antenatal education to check for any abnormalities, texture (firmness and elasticity), inverted or flat nipple, and to discuss any breast surgeries that could affect nursing. Previous breast surgery does not necessarily indicate there will be difficulties with breastfeeding, but careful follow-up may be warranted.
Breastfeeding management at birth
We already established that breastfeeding is a natural process and that your milk is produced whether or not you have gathered all the available resources on nursing. But health care providers and lactation consultants can be instrumental to a successful experience. Mom can benefit from the help of a doula (birth coach) during and after labor. The presence of a doula is known to enhance breastfeeding initiation and duration. Having a doula at your birth can also help you prevent the use of pain-reducing interventions such as epidurals and other medications. These common interventions (also known as intrapartum analgesia) may have an effect on breastfeeding and early milk let-down.
After birth, the healthy newborn should be given directly to mom for skin-to-skin contact until the first feeding is initiated. Extensive and early skin-to-skin contact may increase the duration of breastfeeding. As soon as possible, the baby should be put to the breast (within an hour of birth). This is to be initiated in either the delivery room or recovery room, and every mom should have help ensuring proper breastfeeding technique.
Note that mom and baby rooming-in on a 24-hour basis enhances opportunities for bonding and optimal breastfeeding initiation. Avoid sending your baby to the nursery if at all possible.
At the hospital
Hospital policies and practices influence breastfeeding outcomes by encouraging or discouraging optimal breastfeeding behaviors. If you choose to breastfeed your baby, you should be helped and encouraged to assure a good start. Make sure the hospital staff knows ahead of time about your plan to breastfeed. Getting together: Positioning and Attachment The way you hold your baby to breastfeed may be influenced by cultural or familial traditions. Whatever position you and your baby choose should be comfortable and safe for both of you.
-
Positioning
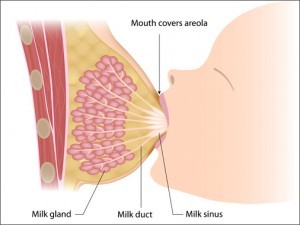
Baby should be in a quiet but alert state. A crying baby needs to be calmed before beginning breastfeeding. A sleepy baby may not respond with a proper rooting reflex and may not take the breast. Unwrapping and undressing a baby—or gently massaging baby’s back or soles of his feet—can help wake baby up. Sit comfortably with your back well supported, and bring baby close to you. Offer the breast to the baby in a way that promotes good attachment of the baby’s mouth to the breast. You can support your breast with all four fingers below and thumb resting lightly at the top of the breast. This is called the “C hold”.

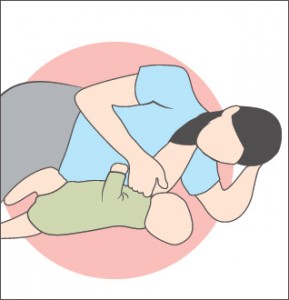
Thumb and fingers should be away from the areola so baby can grasp the nipple and areola without interference. Often, moms are seen offering the breast to the baby using a “scissor hold,” with the nipple between the forefinger and middle finger. If your fingers block the areola, the baby cannot attach properly. Seated in this position, the baby should be held at the same level as your breast, turned so the baby’s abdomen faces your abdomen (tummy to tummy). Hold baby close, and use pillows to help support him. For “baby led” or biological positioning, moms are encouraged to lie backward rather than sit upright. The baby is placed on mom’s chest and allowed to use his reflexes and natural behaviors to find each breast and self-attach.

Below are other common positions for breastfeeding. Find what seems natural and comfortable to both you and your baby.
-
Cradle (cross chest):
The baby across your lap, baby’s head is in the crook of your arm.

-
Modified cradle:
The baby lies across your lap, your opposite arm supports the baby’s back and neck.

-
Side sitting (football hold):
You and baby are sitting up; baby sits facing you with his legs under your arm; your hand supports baby’s back and neck. This position is comfortable after cesarean delivery because the baby’s weight is away from the incision. Sleepy babies may stay awake and feed better in this more upright position.

-
Side-lying:
You and baby lie side by side with your lower arm extended or underneath your head.
-
Attachment
The way the baby grasps the nipple/areola area and pulls it into his mouth for feeding is referred to as “latch.” Your baby’s latch is considered to be the most important factor in preventing problems that lead to premature weaning. Normal-term babies are born with a number of reflexes and behaviors. These reflexes include a rooting reflex that prompts him to open his mouth and turn toward the breast when hungry. A light touch to the middle of the baby’s upper lip will help elicit this reflex. Baby opens his mouth wide and brings his tongue down and forward over the lower gum to pull the nipple into his mouth. A crying baby will need to be calmed since the tongue is usually elevated during crying. When properly attached, baby’s lips are flanged outward over the areola (often called “fishy lips”). Once attached correctly, the baby’s nose just touches the breast, his lips are flanged out, and his chin is against the breast.
Colostrum, baby’s “first immunization,” is a thick, yellowish fluid present in the breast during pregnancy and two to four days after birth. Although seemingly small in quantity (40-50 ml during the first 24 hours), colostrum provides ideal nutrients and immunological substances. It contains much more protein and much less fat and lactose compared to mature milk, and it is rich in vitamin A precursor (beta carotene), which gives colostrum its yellowish color. In the early days of baby’s life, vitamin A is highly important for protection against infections and for early retinal development. White blood cells are also present for further protection against infection. Hunger cues Crying is a late sign of hunger. Breastfeeding should be initiated in response to early hunger cues rather than waiting until the baby cries for milk.
Early hunger cues include:
-
Waking up
-
Bringing hands to his or her mouth
-
Rooting (baby moves head and mouth to look for a nearby nipple)
-
Mouthing movements
Milk requirements in the first 3 days The total colostrum available in the first few days are small (40-50 ml). But it is well matched to the newborn’s small stomach capacity of about 20 ml (about 4 teaspoons). Milk will begin to appear a few days after birth whether you breastfeed or not, but the stimulus of a baby suckling at the breast builds and maintains milk production.
Going home
Unsupportive family members and friends easily undermine a new mom’s confidence. You can ask for help at home in the early days. It is advantageous to mom’s healing and her new breastfeeding relationship if someone else can do housework and errands. With no help, a new mom is at high risk for early weaning since the first couple of weeks can be overwhelming.
Milk requirements by the end of the first week
The frequency of feeding regulates milk supply. The more often a baby nurses, the greater the milk supply. Conversely, a baby who sleeps many hours at a time in the early weeks, or who feeds less than an average of eight times in 24 hours, does not have the opportunity to stimulate the breast. This causes the milk supply to drop. The more demand for milk, the greater the supply.
Frequency and pattern of feedings
Breast milk production are baby driven, meaning normal-term babies indicate when they are hungry and when they are full. Breast milk is easily digested, so your baby signals his need to eat about every two to three hours (sometimes more often), or at least eight times every 24 hours in the early weeks. Some babies cluster their feedings into a particular part of the 24 hours and feed less frequently during the remaining hours of the day.
Weight loss
Newborns usually lose some weight in the first few days. Breastfeeding twins or multiples often lose less weight because their milk comes in so quickly. Babies usually lose 5% of their birth weight during the first few days, while 10% is acceptable if all else is going well. Schedule a follow-up visit to ensure the baby is at a healthy weight and progressing well.
Before your breastfeeding journey begins, gather information and resources to help prepare you. Talk to family and friends who have had positive nursing experiences, and seek out a lactation consultant and/or doula who can commit to helping you establish a healthy breastfeeding relationship from the very beginning.
But also take a deep breath; being a mom is so much more than head knowledge. Plan for many unexpected moments in early parenting, and decide to treasure the journey no matter what it brings or how prepared you do or don’t feel. You’re gonna do great, mama.